The cervical region represents a highly vulnerable anatomical zone and constitutes the second most frequent complaint among our patient cohort. The seven cervical vertebrae are arranged in close apposition, permitting the passage of critical neurovascular structures including spinal nerves, vertebral arteries and venous plexuses through their intervertebral foramina. Cumulative occupational stresses, postural maladaptations and repetitive microtrauma sustained over the course of one’s professional activities often precipitate symptomatic cervical dysfunction.
Patients may report paresthesiae—classically described as “pins and needles” or burning dysaesthesia—most often attributable to radicular compression at the neuroforaminal exit zone. Such impingement commonly arises from intervertebral disc protrusion or osteophytic encroachment secondary to degenerative spondylosis.
Migraines constitute a moderate‑to‑severe, often unilateral, throbbing cephalalgia, believed to arise from aberrant cortical neuronal activity such as cortical spreading depression provoking transient dysregulation of neurovascular and neurochemical pathways within the cranium.
These attacks reflect perturbations in neurotransmitter release and cerebral blood‑vessel tone.
Individual susceptibility is modulated by discrete precipitating factors hormonal fluctuations, psychosocial stressors, dietary constituents, and the like whose specific influence varies person to person.
A thorough evaluation to delineate each patient’s unique trigger profile is therefore indispensable for targeted prophylaxis and acute management.
Virtually the entire population will experience lumbalgia at some juncture sufficient to impair occupational performance, activities of daily living or leisure pursuits. Globally, spinal pain ranks second only to cephalalgia among neurological disorders.
Acute low back pain predominantly mechanical in origin typically subsides within days to weeks.
By contrast, pain persisting beyond three months fulfils the definition of chronic lumbosacral pain.
Chronic presentations often exhibit a progressive course, and identification of a singular aetiological factor can be elusive.
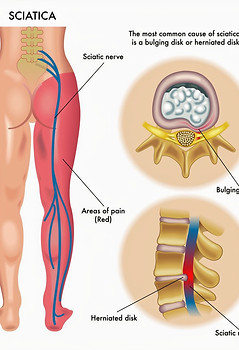
Sciatica frequently engenders profound disability and a premature sense of frailty. Pathophysiologically, it reflects neuropathic irritation of the sciatic nerve typically precipitated by an inflammatory cascade secondary to mechanical compression. Common compressive aetiologies include intervertebral disc herniation with neuroforaminal encroachment, facet joint arthropathy, hypertonicity of the deep gluteal musculature, vertebral subluxation, pelvic rotation or sacro‑iliac joint dysfunction.
The sciatic nerve: the body’s most substantial and longest peripheral nerve originates in the lumbosacral plexus and extends distally into the foot.
Although patients often seek a singular culprit, sciatica usually represents a multifactorial syndrome in which segmental misalignment coexists with soft‑tissue contracture, inflammatory mediators and altered biomechanics.